The incidence of tuberculosis (TB) is dropping in the US, but the World Health Organization (WHO) considers it to be epidemic in the rest of the world — there were over 10 million new cases in 2016.
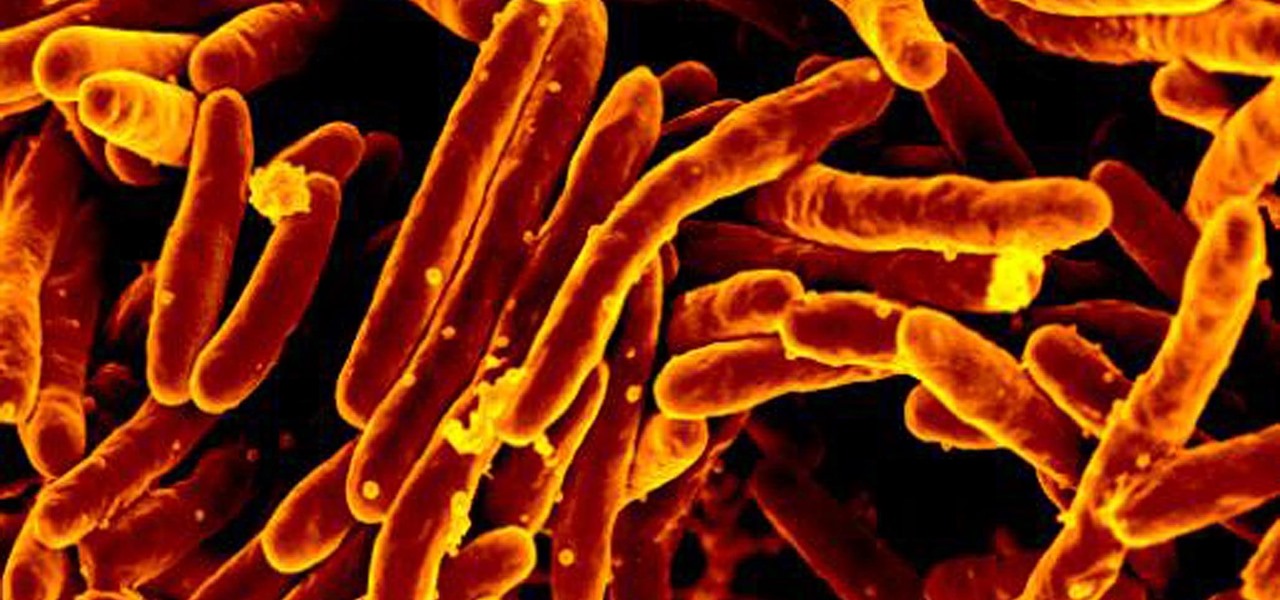
The bacteria that causes TB, Mycobacterium tuberculosis, is rapidly becoming resistant to several drugs used to treat the infection. Three drugs — fluoroquinolones — are often used to treat drug-resistant TB and treatment can take up to half a year. However, there hasn't been any way to tell whether one might treat an infection better than the others. Now, using a computer model to simulate a TB infection, researchers have been able to predict the effect of the three drugs on the bacteria.
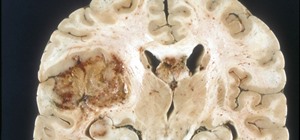
Our bodies try to contain TB bacteria in granulomas, clusters of host cells and bacteria that develop in the lungs of tuberculosis patients. Study researcher Elsje Pienaar and colleagues at the University of Michigan in Ann Arbor and Rutgers developed a computer model to simulate the effects of the three drugs on granulomas. They showed that one fluoroquinolone, moxifloxacin, may be superior to the other two.
Their findings were published August 17 in PLOS Computational Biology.
"The exciting thing about this study is that we are able [to] perform a side-by-side comparison of fluoroquinolones in identical infections. The potential practical application of our findings is to guide selection of individual fluoroquinolones for tuberculosis treatment," said Pienaar in a press release from PLOS.
Latent and Active Tuberculosis
Tuberculosis, caused by the bacteria Mycobacterium tuberculosis, spreads from one person to another. When an infected person coughs or speaks, they spew bacteria into the air, where they are inhaled by others nearby. The bacteria can cause disease in almost any part of the body, including the brain, kidneys, and spine.
However, not everyone who becomes infected has symptoms of the disease. That's because most people develop a latent infection. People with latent TB, don't have symptoms, are not infectious, and cannot spread it to others. The only way someone with latent TB might realize it is if a TB skin or blood test turns up positive.
In a latent infection, the body isolates TB bacteria in granulomas — dense pockets of immune white blood cells, bacteria, and dead cells that contain the infection and limit the growth of the bacteria, but don't kill it. Unfortunately, granulomas also provide a little niche where the bacteria can survive and later spread out to cause an active infection.
Without treatment, about five to 10% of people with the latent disease will develop active TB at some point; half of those will do it in the first two years of infection.
People with active TB may have a bad cough for several weeks, pain the chest, cough up blood, or experience weakness. They may lose weight, lack appetite, have fever or chills, and have night sweats.
People with active TB are treated with combinations of isoniazid, rifampicin, and rifapentine. The Centers for Disease Control and Prevention reported that about 10% of the TB in the US was drug-resistant in 2011.
Moxifloxacin, levofloxacin, and gatifloxacin are three fluoroquinolones prescribed for treating drug-resistant TB. The WHO recommends levofloxacin over moxifloxacin, and moxifloxacin over gatifloxacin, but there haven't been any clinical trials that show one drug kills the bacteria better than the others. Pienaar and her colleagues used a computer model that simulated granuloma formation and function, along with drug concentrations at the granulomas to predict which fluoroquinolone would perform best.
Modeling an Infection
The research team used a computer simulation model called GranSim to perform their study. They also performed some lab experiments to get data for their simulation. TB bacteria was also mixed with different concentrations of the drugs to see how much was needed to kill the bacteria. White blood cells called macrophages from mice were infected with TB bacteria and exposed to different concentrations of the different fluoroquinolones, to get data on how a range of drug concentrations made their way into cells. The scientists also treated TB infected rabbits with the antibiotics and analyzed concentrations of drugs in their plasma at different times and drug distribution between granulomas.
The model created a simulation of granuloma formation and function, incorporating several different factors:
- White cell movement into the granuloma.
- The secretion and diffusion of chemokines and cytokines (chemicals secreted by the white cells that signal immune responses).
- The growth of TB bacteria present.
- Bacterial killing by macrophages in the granulomas.
GranSim also used the results of the lab experiments using the drug to create their models.
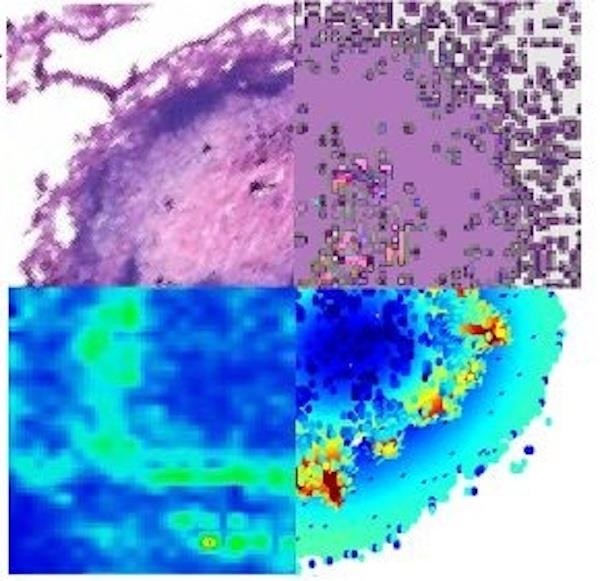
In the simulations, moxifloxacin killed bacteria in granulomas more quickly than the other two drugs, and it performed better when the simulated patients missed doses. Levofloxacin killed bacteria quicker gatifloxacin. Moxifloxacin and levofloxacin killed more bacteria in granulomas than gatifloxacin, but none of the three drugs were able to kill bacteria at the very center of the granulomas.
The study authors concluded that moxifloxacin has a small, but potentially clinically significant, advantage over levofloxacin and levofloxacin performed better than gatifloxacin. Interestingly, this drug sequence is different than one the WHO recommends. They wrote that this approach, which combines experimental and computational methods, can guide antibiotic selection for TB.
The computer simulation predictions are now being tested in animal experiments. The team is also running simulations of fluoroquinolones compared to other tuberculosis drugs. Results of those investigations will bring us one step closer to narrowing down the best possible drug combinations for tuberculosis treatment.
Just updated your iPhone? You'll find new emoji, enhanced security, podcast transcripts, Apple Cash virtual numbers, and other useful features. There are even new additions hidden within Safari. Find out what's new and changed on your iPhone with the iOS 17.4 update.























Be the First to Comment
Share Your Thoughts